Arthritis of the Foot and Ankle
Source: American Academy of Orthopedic Surgeons
Synopsis
There are more than 100 different types of arthritis. But when most people talk about arthritis, they are usually referring to the most common form, osteoarthritis ("osteo" means bone). Osteoarthritis develops as we age and is often called "wear-and-tear" arthritis. Over the years, the thin covering (cartilage) on the ends of bones becomes worn and frayed. This results in inflammation, swelling, and pain in the joint.
An injury to a joint, even if treated properly, can cause osteoarthritis to develop in the future. This is often referred to as traumatic arthritis. It may develop months or years after a severe sprain, torn ligament or broken bone.
Anatomy & Function
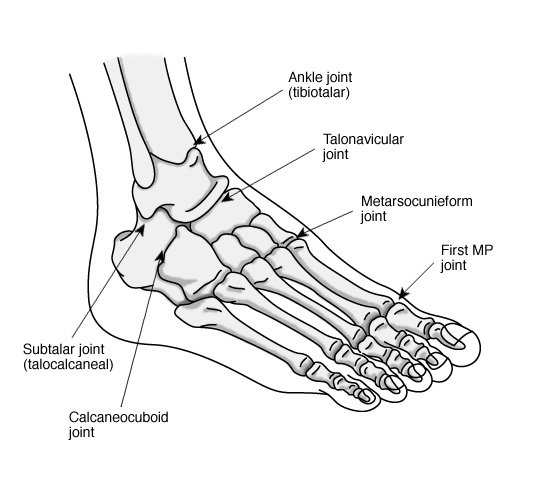
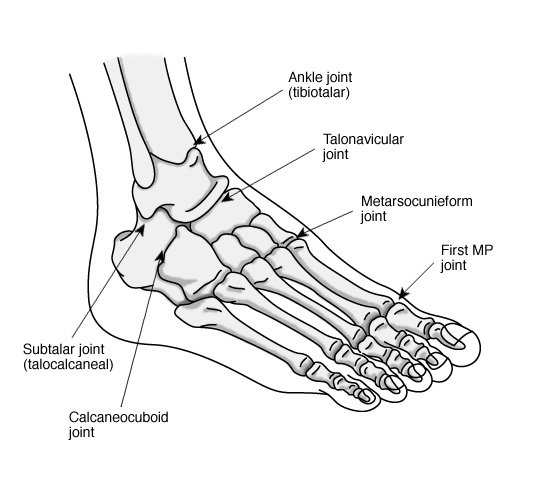
There are 28 bones and over 30 joints in the foot. Tough bands of tissue, called ligaments, hold the bones and joints in place. If arthritis develops in one or more of these joints, your balance and walk may be affected. The foot joints most commonly affected by arthritis include:
the ankle (tibiotalar joint), where the shinbone (tibia) rests on the uppermost bone of the foot (the talus)
the three joints of the hindfoot: the subtalar or talocalcaneal joint, where the bottom of the talus connects to the heel bone (calcaneus); the talonavicular joint, where the talus connects to the inner midfoot bone (naviculus) and the calcaneocuboid joint, where the heel bone connects to the outer midfoot bone (cuboid)
the midfoot (metatarsocunieform joint), where one of the forefoot bones (metatarsals) connects to the smaller midfoot bones (cunieforms)
the great toe (first metatarsophalangeal joint), where the first metatarsal connects to the toe bone (phalange); this is also where bunions usually develop
Signs and symptoms
Signs and symptoms of arthritis of the foot vary, depending on which joint is affected. Common symptoms include pain or tenderness, stiffness or reduced motion, and swelling. Walking may be difficult.
Diagnosing arthritis of the foot and ankle
Your doctor will begin by getting your medical history and giving you a physical exam. Among the questions you may be asked are:
When did the pain start? Is it worse at night? Does it get worse when you walk or run? Is it continuous, or does it come and go?
Have you ever had an injury to your foot or ankle? What kind of injury? When did it occur? How was it treated?
Is the pain in both feet or just one? Where is the pain centered?
What kinds of shoes do you normally wear? Are you taking any medications?
Your doctor may do a gait analysis. This shows how the bones in your leg and foot line up as you walk, measures your stride, and tests the strength of your ankles and feet. You may also need some diagnostic tests. X-rays can show changes in the spacing between bones or in the shape of the bones themselves. A bone scan, computed tomography (CT) scan, or magnetic resonance image (MRI) may also be used in the evaluation.
Treating your arthritis
Depending on the type, location and severity of your arthritis, there are many types of treatment available. Nonsurgical treatment options include:
Taking pain relievers and anti-inflammatory medication to reduce swelling
Putting a pad, arch support or other type of insert in your shoe
Wearing a custom-made shoe, such as a stiff-soled shoe with a rocker bottom
Using an ankle-foot orthosis (AFO)
Wearing a brace or using a cane
Participating in a program of physical therapy and exercises
Controlling your weight or taking nutritional supplements
Getting a dose of steroid medication injected into the joint
If your arthritis doesnít respond to such conservative treatments, surgical options are available. The type of surgery thatís best for you will depend on the type of arthritis you have, the impact of the disease on your joints, and the location of the arthritis. Sometimes more than one type of surgery will be needed. The primary surgeries performed for arthritis of the foot and ankle are:
Arthroscopic debridement. Arthroscopic surgery may be helpful in the early stages of arthritis. A pencil-sized instrument (arthroscope) with a small lens, a miniature camera and a lighting system is inserted into a joint. This projects three-dimensional images of the joint on a television monitor, enabling the surgeon to look directly inside the joint and identify the trouble. Tiny probes, forceps, knives and shavers can then be used to clean the joint area by removing foreign tissue and bony outgrowths (spurs).
Arthrodesis, or fusion. This surgery eliminates the joint completely by welding the bones together. Pins, plates and screws or rods through the bone are used to hold the bones together until they heal. A bone graft is sometimes needed. Your doctor may be able to use a piece of your own bone, taken from one of the lower leg bones or the hip, for the graft. This surgery is normally quite successful. A very small percentage of patients have problems with wound healing. These complications can be addressed by bracing or additional surgery.
Arthroplasty, or joint replacement. In rare cases, your doctor may recommend replacing the ankle joint with artificial implants. However, total ankle joint replacement is not as advanced or successful as total hip or knee joint replacement. The implant may loosen or fail, resulting in the need for additional surgery.
Outcomes and rehabilitation
Initially, foot and ankle surgery can be quite painful, so you will be given pain relievers both in the hospital and after you are released. After surgery, you will have to restrict activities for a time. You may have to wear a cast and use crutches, a walker, or a wheelchair, depending on the type of surgery you had. Keeping your foot elevated above the level of your heart will be very important for the first week or so.
You will not be able to put any weight on your foot for at least four to six weeks, and full recovery takes four to nine months. You may also need to participate in a physical therapy program for several months to regain strength in the foot and restore range of motion. Usually, you can return to ordinary daily activities in three to four months, although you may have to wear special shoes or braces. In the vast majority of cases, surgery brings pain relief and makes it easier for you to do daily activities.