Posterior Tibial Tendon Disfunction (Insuffency, Posterior Tibial Tendonitis)
Anatomy & Function
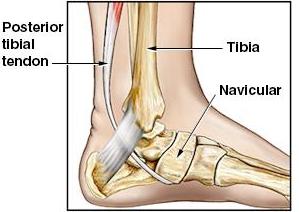
An acquired flatfoot deformity usually occurs when the posterior tibial tendon fails to function properly. The posterior tibial tendon lies within the calf of the foreleg. The tendon passes behind the medial malleolus of the ankle and attaches to a bone in the foot called the navicular bone.
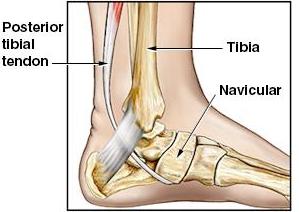
Figure 1:
Normal anatomy and arch as seen in this view of the left ankle from the medial
side.
The navicular bone is a key structural component in the formation of the arch of the foot. When this bone is in the proper position, the arch is maintained. However, if this bone moves out of position, towards the bottom of the foot (plantar surface), then the arch begins to sag and disappear. As this occurs, the patient develops a flatfoot deformity.
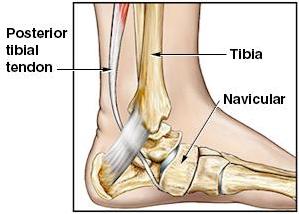
Figure 2:
Abnormal anatomy and falling arch as seen in this view of the left ankle from
the medial side. Compare position of navicular bone in figure 1 with figure 2.
The posterior tibial tendon is essential to the normal functioning of the foot by maintaining the navicular bone in the proper position. By doing so, the arch of the foot is maintained. However, if the posterior tibial tendon fails to function properly, the navicular bone begins to drop, the arch falls and a flatfoot deformity begins to develop. When this occurs, the foot may develop pain with weight bearing.
The posterior tibial tendon injuries appear to fall into 2 categories: traumatic and degenerative. A traumatic injury usually occurs suddenly, as with a blow to the medial side of the ankle or with a twisting injury that results in a complete or partial tear of the tendon. A chronic tear develops over a period of time and is usually related to a slowly developing degenerative tearing (or stretching) of the tendon. When the tendon is damaged, the damage may result in a complete tear, a partial tear, or a stretching type of injury that allows the tendon to remain in one piece, but it becomes functionally too long, and thereby loses the ability to perform properly.
Predisposing factors to degenerative posterior tibial tendon insufficiency (tearing) include: diabetes mellitus, hypertension, obesity, trauma or surgery to the medial aspect of the ankle and steroid injections. In addition, other inflammatory conditions such as rheumatoid arthritis, seronegative arthropathy and infection may also lead to degeneration of the posterior tibial musculotendinous unit.
The chronic degenerative tear of the posterior tibial tendon usually occurs in a patient who is a female, 40+ years of age, without a history of injury, and who does prolonged periods of standing and walking. Lack of proper supporting shoes (Flip Flops,) may also contribute to PTTI as they break down and offer almost no support to the arch of the foot.
Regardless of injury type There are three commonly accepted stages of the adult acquired flatfoot:
| Stage I: | Inflammation and swelling of the posterior tibial tendon around the inside of the ankle. |
| Stage II: | Visible deformity comparing one foot to the other, as the symptomatic foot becomes flatter and more deformed. The deformity is movable and correctable in this stage. |
| Stage III: | The foot progresses to a rigid, non-movable flat foot deformity that is painful, primarily on the outside of the ankle |
Exam and Diagnosis
The physical exam consists of examination of the ankle for areas of swelling, tenderness, and abnormal positioning of the foot, arch, and medial aspect of the ankle. In addition, attention is paid to the forefoot and to the position of the heel. Palpation of the posterior tibial tendon allows for localization of the pain to the tendon, for identification of localized swelling in and around the tendon, and for palpation of the tendon to determine if a gap in the tendon can be felt.
Performing a single limb toe raise and checking the ability of the patient to stand on his/her toes tests the strength of the PTT.
Inspection of the foot allows for identification of abnormal positioning of the forefoot and toes, the medial aspect of the ankle, and the position of the heel. In addition, it is also possible to check the arch height. When doing these tests, they must be performed in the weight bearing position with the patient standing in bare feet.
One of the classic signs of posterior tibial tendon insufficiency is a "splaying" of the forefoot. This means that the medial aspect of the ankle rolls to the inside causing increased prominence of the medial malleolus. At the same time, as the arch drops, the forefoot moves to the outside (laterally). When this occurs, the abnormality is best seen by viewing the patient's feet while the patient is standing. When viewed from the backside, the affected foot will appear to turn to the outside and "too many toes will be seen".

Figure 1: In this figure, the left side is normal and the right side (red markings) is abnormal. As viewed from the backside, the inside of the right ankle (medial side) appears to roll toward the opposite ankle (red arrow). At the same time, both the 4th and 5th toes may be seen on the right (red circle), while only the 5th toe may be seen on the left foot (blue circle).
Although the tendon cannot be seen on x-ray, alteration in the normal position of the bones of the foot may be seen. The MRI scan is an excellent way of visualizing the tendon to identify tendonitis, partial tears, or complete tears. Unfortunately, like most medical tests, the MRI is not 100% accurate.
Treatment
Posterior tibial tendonitis represents an inflammation of the posterior tibial tendon. Initially, in degenerative injuries, the tendon starts out with an area of inflammation, which then begins to degenerate. As it deteriorates, the tendon may begin to have microscopic tearing. This results in a structural weakening of the tendon. As the tendon weakens, it begins to stretch out, causing further tearing. During this process, the area around the tendon becomes painful and swollen. As the tendon stretches and weakens, it becomes unable to support the arch of the foot. As the arch decreases, the normal relationship between the bones of the foot changes. This allows the arch to collapse, which further stretches the tendon causing more damage and tearing. At this point, the medical description of the injury is called: posterior tibial tendonitis, dysfunctional posterior tibial tendon, partial tear of the PTT, or a tear in continuity of the PTT. Without proper treatment, or sometimes, even with proper treatment, the damage is so advanced that healing fails to occur and the tendon ruptures.
The treatment options in this disease process include both operative and several different types of operative treatment. The choice of treatment usually depends on how long the problem has been going on and on the response of the patient to a particular type of treatment. Initially, treatment often consists of physical therapy, icing, NSAID, and activity restriction. Sometimes orthotics are used initially. Occasionally, it is necessary to use a cast.
In more severe situations, or if the problem fails to improve with non-operative treatment, then surgery may be indicated. Usually this consists of some type of reconstruction/repair of the PTT. In more advanced cases, it is necessary to fuse the bones of the foot together to reestablish the normal relationship of the bones of the foot to each other.