
Osteochondritis Dissecans -Talus
Anatomy & Function
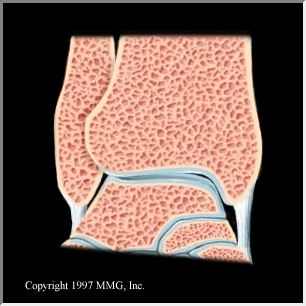
The ankle is a joint which is formed by the tibia and fibula (bones above the ankle in the foreleg) and the talus (below the ankle joint). The ankle joint allows for the upwards (dorsiflexion) and downwards (plantarflexion) motion. The end of the shin bone (tibia) forms the inner bony prominence of the ankle called the medial malleolus. The outer bony prominence is called the lateral malleolus and is formed by the small outer bone in the foreleg called the fibula.

Osteochondritis dissecans is an injury to the talus bone of the ankle joint. Because the ankle joint is so small, the amount of force that goes across the joint, with each step, has been estimated to be approximately 5-10 times a person's body weight.As a result of this tremendous force that occurs in the ankle joint, relatively small injuries to the articular surface of the talus often result in chronically painful injuries.
Osteochondritis dissecans is the result of the isolated loss of blood flow to a portion of the talus bone. Usually this occurs in conjunction with a history of trauma. It is sometimes also known as an osteochondral fracture of the talus, chip fracture of the articular surface or a chondral fracture of the talus.
The development of osteochondritis may be very slow. Initially, a person may sustain a twisting injury to the ankle. As the ankle is injured, the talus bone twists within the space between the tibia and fibula. As this twisting occurs, the ligaments around the ankle may be stretched . Unfortunately, in some people, as the twisting injury occurs, not only are the ankle ligaments stretched, but the talus bone strikes the tibia or fibula. When this occurs, some type of injury to the talus, tibia, or fibula happens. Typically, the majority of the damage occurs to the talus at the articular surface.
The articular surface is normally nice and smooth. It has no blood supply. Without a blood supply, the potential for healing damage to the articular cartilage is minimal. Therefore, when this tissue is damaged, it may slowly deteriorate with the passage of time. As the articular surface deteriorates, the surface changes from a nice smooth frictionless surface to a rough cobblestone like surface. This rough degenerative surface is a form of arthritis.
When the ankle is twisted, and the talus impacts the tibia or fibula, the talar articular surface may be merely bruised, or a more serious injury may occur. If the twisting injury results in a shearing force to the talus as it impacts the tibia orfibula, then a chip fracture may occur. This "chip fracture" may either be complete, or incomplete, and it may be detached (loose body), partially detached, or non-displaced.
To further confuse things, the bone injury may not become visible on x-ray for several months.
When the chip becomes detached, then it floats freely inside the ankle joint. When this occurs, patients may develop a definite catching sensation that is associated with a loss of motion. In addition, the joint may become swollen and painful. Later, when the chip slips out of the way, the symptoms may improve, swelling decrease, and the may disappear - only to reappear at another time.
If the fragment is partially detached, then similar problems may occur.
However, if the fragment is not detached, then the only complaints may be pain and discomfort.
The location of the injury is on the articular surface of the talus. It may be located on either side of the talar dome. The talar dome is that semicircular portion of the talus that sits beneath the tibia. On this dome, the osteochondritis dissecans may occur on either the medial or lateral sides of the talar dome (articular surface of the talus).
Diagnosis
Initially, a physical exam should be done to try to
determine the site of tenderness and the cause of the patient's complaint.
During this process, the stability of the ligaments and tendons around the ankle
is usually checked along with the range of motion of the joint. Palpation is used
to determine the areas of tenderness and to check for signs of an effusion
(collection of fluid within the joint).
Sometimes, it is necessary to aspirate (remove) the joint
fluid collection to determine the type of fluid present. IF the fluid is bloody
with fat globules present (lipohemarthrosis), then some type of injury to the
bone may be the cause.
X-rays are taken to evaluate the talus, tibia, and fibula. With the x-rays, it is possible to check for signs of arthritis, loose bodies, chip fractures, fractures, and other bone abnormalities. Unfortunately, because the ankle bones overlap onx-rays, it is necessary to take multiple views from different angles in order to try to completely evaluate the bones. Even with multiple views, it is still possible for the overlapping bone images to hide abnormalities. For that reason, if patients fail to improve, it is often necessary to obtain more sophisticated imaging studies such as MRIs, CT scans, bone scans, or tomograms. Unfortunately, none of these studies are 100% accurate.
With Osteochondritis, sometimes, the initial imaging
studies are normal. Only by repeating the imaging studies is the abnormality
ever found. This is related to the fact the Osteochondritis may take time to
develop. Initially, the damage may be great enough to cause very mild
intermittent symptoms, but too small to be visualized on x-ray. With the passage
of time, as the Osteochondritis worsens, then changes begin to appear on the
imaging studies.
Imaging Studies
The classification of osteochondritis dessicans is important because the prognosis (expected outcome) and treatment options are often linked to the severity of the osteochondritis dessicans. Typically, the injury classification is from stage 1through stage 4. As the severity of the injury progresses, the stage increases with stage 4 osteochondritis dissecans being the worst. Although the classification is often based upon the x-ray appearance, the abnormalities noted on x-ray may not always be completely accurate.
In the following series of drawings, the ankle has undergone a twisting injury the results in the progressive stretching of the medial ankle ligament (deltoid ligament). By stage 2, the ligament has torn. As the twisting force is applied to the talus, the articular surface of the talus hits the tibia. A this occurs with progressively greater force, the talus bone sustains progressively greater damage as indicated by the development of a bigger fracture line and eventually a loose body (bonechip, osteochondral fragment),
Stage 1: This is the most minor abnormality. Typically,
there has been an injury to the articular surface of the talus. Although an
injury has occurred to the articular surface, no significant disruption of the
bone has taken place.
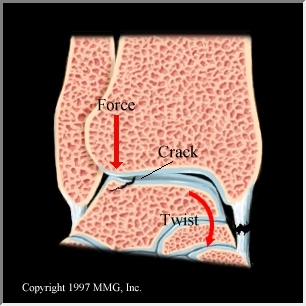
Stage 2: As the injury
increases, a hairline crack begins
to appear in the talus, just beneath the articular surface. The crack (or
fracture line) is incomplete. This means that it does not completely extend from
one side of the injury to the other side.
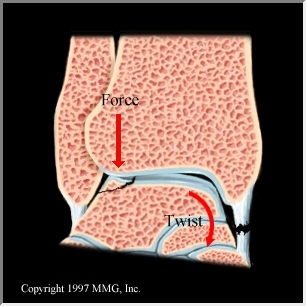
Stage 3: The incomplete fracture line has now progressed
to completely separate the fragment. However, the fragment remains in its place
on the surface of the talus.
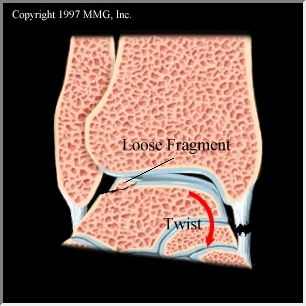
Stage 4: Now the fragment has broken loose and changed position so that it is no longer in the defect on the talus.
Treatment
The treatment depends on the age of the patient, the circumstances of the injury, and the type of bone damage. A simple bone contusion (bruise) would be treated differently then a detached bone fragment. The treatment options may vary from simply being on crutches to being casted to having surgery. The surgical procedures used to treat osteochondritis dissecans may involve removing the fragment, attempting to reattach the fragment, drilling the underlying bone to promote blood flow, or some combination of these procedures. Obviously, the exact treatment and procedure needs to be individualized to the patient, the type of bone injury, and the location of the bone injury.